"Ultrasound is very important for tumor resection because of brain shift and the need to see residual tumor and the tumor border."
Recently, we introduced you to Prof. Geirmund Unsgård, Professor Emeritus of Neurosurgery at the Norwegian University of Science and Technology (NTNU). We have talked with Prof. Unsgård about using intraoperative ultrasound in neurosurgery and how the use of intraoperative ultrasound can help account for brain shift during neurosurgery. Today, we are talking with Professor Unsgård about the visualization and planning of tumor resection surgeries.
Visualization and Planning of Tumor Resection
According to Prof. Unsgård, visualization of the tumor beyond the surface of the tissue during a neurosurgical procedure is only made possible by real-time, intraoperative ultrasound. Real-time intraoperative ultrasound offers reliable visualization of brain tumors and helps guide tumor resections. “Ultrasound is very important for tumor resection because of brain shift and the need to see residual tumor and the tumor border,” says Prof. Unsgård.
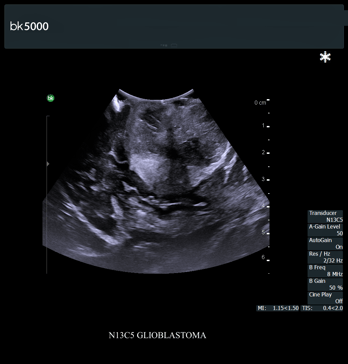 Glioblastoma with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Glioblastoma with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Tumor Resection Procedure
Prof. Unsgård recommends using intraoperative ultrasound for repeated scans during tumor resection surgery. This provides surgeons with real-time information about extent of resection. During tumor resection, Prof. Unsgård uses intraoperative ultrasound for:
- After the craniotomy, intraoperative ultrasound can be used through the dura to get acquainted with the lesion and how it looks on ultrasound.
- After the dura is opened, the next scan can be taken, and this becomes the basis for the resection.
- The surgeon can then go ahead based on the information in the ultrasound image and carry out the resection.
- Another ultrasound acquisition can be taken. If some tumor tissue remains, the surgeon can then continue to resect.
Prof. Unsgård uses intraoperative ultrasound in an average of seven or eight times during one operation.
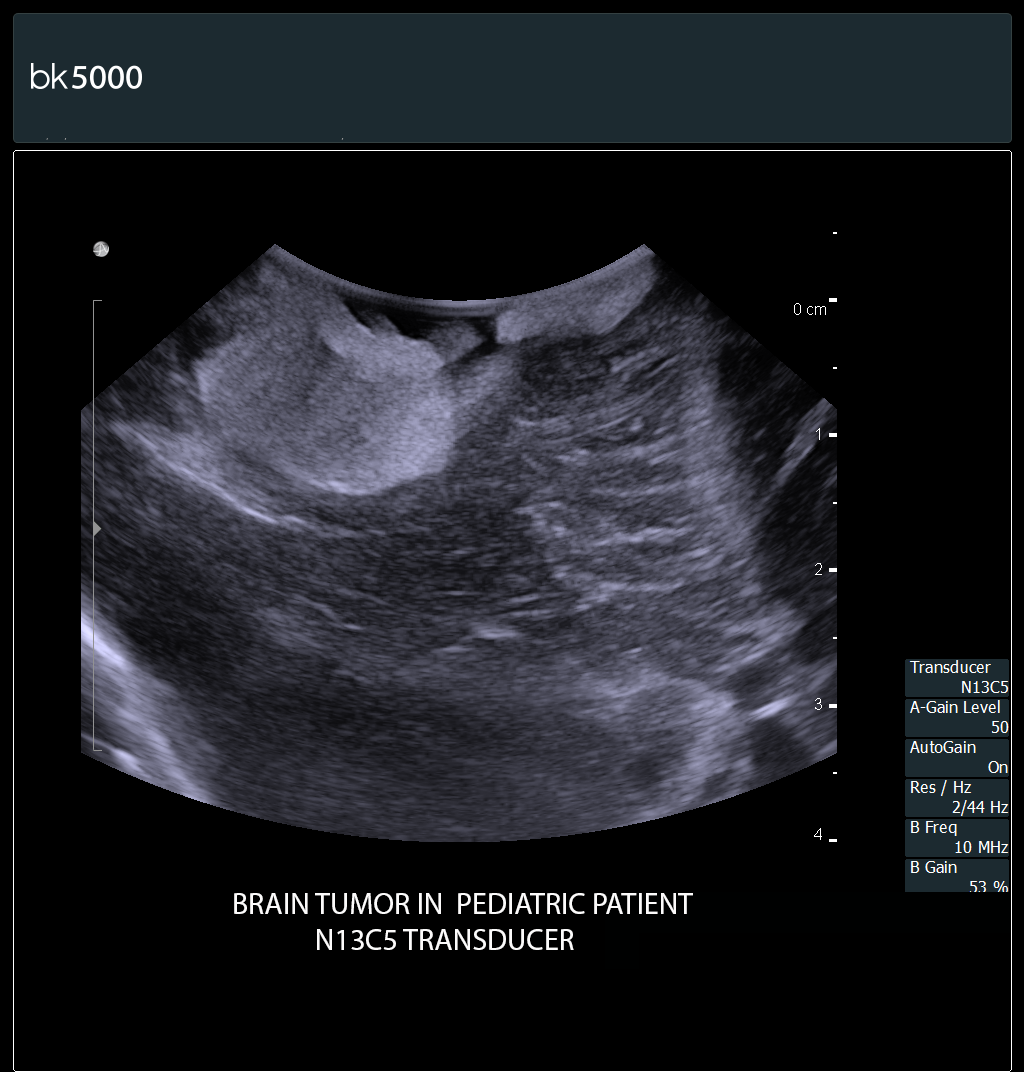 Pediatric brain tumor with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Pediatric brain tumor with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Using Color Doppler to Avoid Harm to Blood Vessels
“As a neurosurgeon, you do have to be very cautious not to damage blood vessels,” says Prof. Unsgård. Color Doppler, Power Doppler, and Pulse Wave Doppler are available on BK Medical’s bk5000 intraoperative ultrasound system. These modes enable visualization of blood flow location and direction. This is important when, for example, a surgeon is resecting an insular glioma. “The surgeon will need to be able to visualize the exact location of the insular arteries,” says Prof. Unsgård. “Power Doppler imaging during intraoperative ultrasound helps surgeons to visualize the lenticulostriate vessels, which are crucial vessels to the pyramidal tracts, and must be avoided during tumor surgeries.”
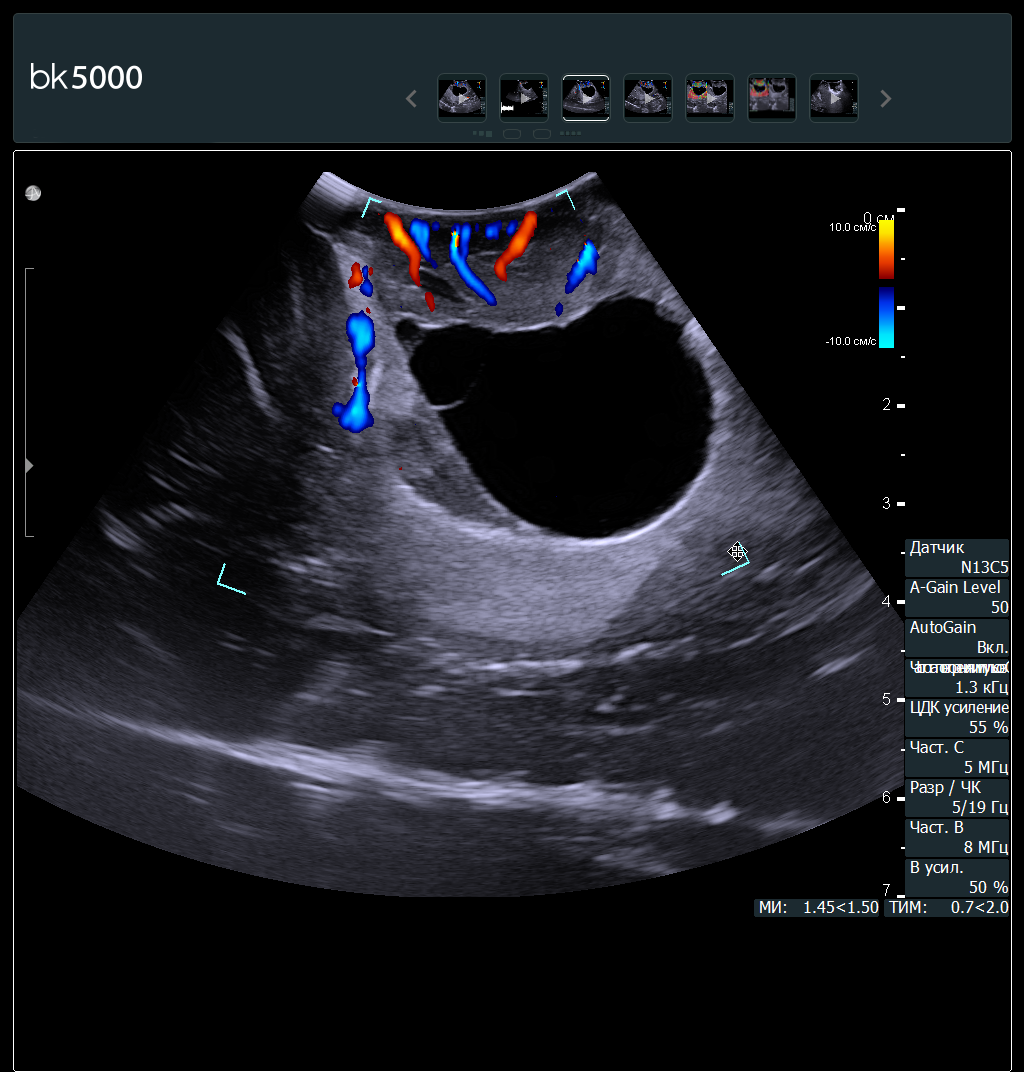 Brain tumor with color Doppler, with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Brain tumor with color Doppler, with BK Medical’s bk5000 intraoperative ultrasound system and craniotomy transducer (N13C5)
Brain Shift and Tumor Resection
Intraoperative ultrasound can also be used to account for brain shift during tumor resection. Current ultrasound technology provides detailed visualization of the true location of the tumor and nearby structures of the brain, helping the surgeon to account for brain shift and update the surgical plan intraoperatively. “To perform a successful resection, you must be able to see the tumor border and residual tumor at their true locations,” he says.
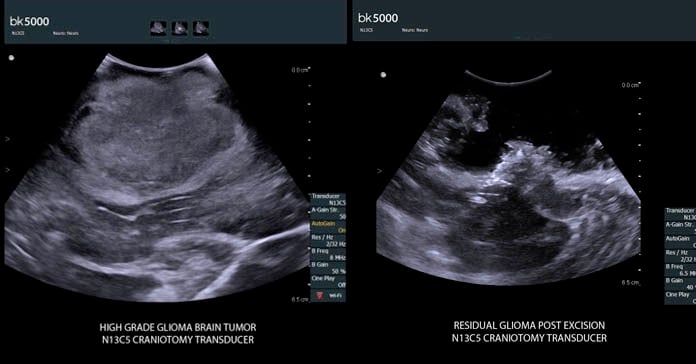 These ultrasound images, from the same case, show, on the left, a high grade glioma; on the right, residual tumor post excision. Both images with BK Medical’s bk5000 ultrasound system and craniotomy transducer (N13C5).
These ultrasound images, from the same case, show, on the left, a high grade glioma; on the right, residual tumor post excision. Both images with BK Medical’s bk5000 ultrasound system and craniotomy transducer (N13C5).
“By visualizing a tumor at its true location, surgeons can potentially remove more problematic tissue than they would if not using intraoperative ultrasound,” says Prof. Unsgård. “I plan for the use of ultrasound in every tumor operation.”

