There is a better chance of successful treatment of prostate cancer when it is detected early and confined to the prostate gland.1 Increasingly, multiparametric MRI (mpMRI) is being recommended before biopsy as part of a prostate cancer pathway.2 Compared with TRUS-biopsy, mpMRI has significantly better sensitivity and negative predictive value for clinically important prostate cancer.2 If used as a triage test before first prostate biopsy, mpMRI could reduce unnecessary biopsies by a quarter; mpMRI could also reduce over-diagnosis of clinically insignificant prostate cancer and improve detection of clinically significant cancer.2
MRI/ultrasound fusion biopsy is an advanced technique for performing biopsies that is being used increasingly to improve the accuracy of prostate biopsy.3 Fusing real-time ultrasound images with pre-exam MRI data provides better guidance to help accurately target lesions identified on the MRI, potentially reducing the risk of missing high-grade tumors or under-staging tumors during active surveillance. This is an improvement over the traditional biopsy method, in which biopsies are taken with random sampling, making it possible that a biopsy could miss cancerous cells in the prostate.
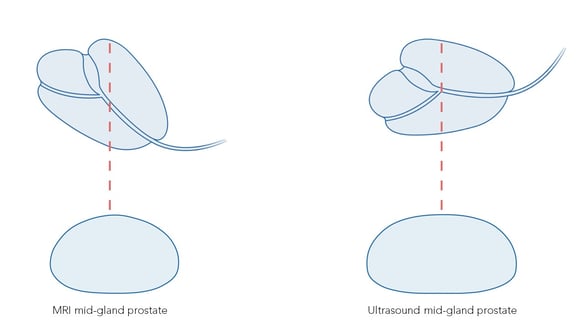
The primary challenge of all MRI/ultrasound fusion biopsy systems is that MRI exams are taken with the patient in the supine position, while biopsies are typically performed in either the left lateral decubitus (LLD) position for transrectal scans or the lithotomy position for transperineal scans. Due to the differences in patient positioning, the prostate will appear differently on MR and ultrasound images.
BK Medical Uses Predictive Fusion®
To manage these differences in patient positioning, MRI/ultrasound fusion biopsy systems incorporate either elastic registration or rigid registration. The bkFusion workflow uses a type of rigid registration and a unique algorithm called Predictive Fusion®.
Elastic Registration
Elastic registration—also called deformable registration—attempts to maximize the alignment of MRI images to ultrasound images through local deformation, translation, and rotation. As a result, elastic registration may result in the distortion of true anatomy in the images. In fact, one study concludes that, in the case of inexperienced users, elastic registration may actually produce increased registration error.4 With elastic registration, the anatomy is artificially altered by the computer in order to create the appearance of a match,5 and the clinician cannot visually see any registration errors that may occur.
Rigid Registration
Rigid registration—also called non-deformable registration—attempts to minimize image distortion when registering the MRI to the ultrasound image. It does this through translation and rotation of images, but does not create local deformations. Instead, rigid registration maintains the true anatomical shape and locations of the prostate in the images. To account for local registration errors, the operator manually adjusts the alignment of real-time ultrasound and MRI images. Whereas with elastic registration the registration errors cannot be seen, with rigid registration the clinician can visually see any errors and can therefore make their own decisions at the time of biopsy. Rigid registration has been shown to decrease registration errors when targeting lesions at the edge of the prostate.6
What Is Predictive Fusion®?
The bkFusion MRI/ultrasound fusion biopsy workflow utilizes rigid registration. It also incorporates a unique algorithm called Predictive Fusion® to orient the supine MRI before the patient’s procedure. In this way Predictive Fusion® reverses the registration process, reorienting the supine MRI to match the prostate biopsy orientation, helping the clinician reduce uncertainty and correct registration errors before they are made, and before a patient’s procedure.
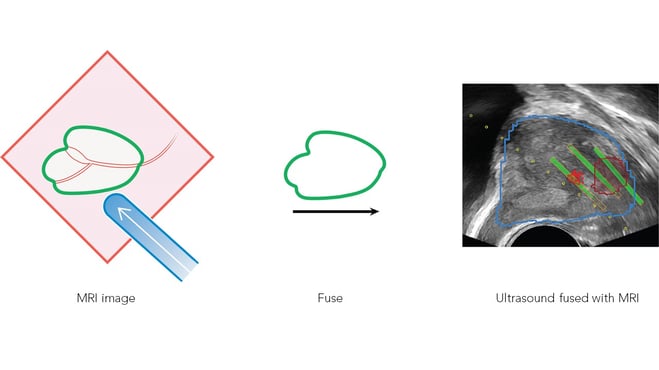
When the biopsy begins, the reoriented prostate MRI contours are overlaid on the real-time ultrasound image, at which time the clinician can correct for any registration uncertainty, realigning and making micro-adjustments without the need to conduct additional ultrasound sweeps. Contouring and segmentation on the ultrasound image are not required, allowing the urologist to follow a familiar biopsy workflow.
For additional information about bkFusion and Predictive Fusion®, read more here.
[1] https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087
[2] Ahmed HU, Bosaily AE-S, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. The Lancet. 2017;389(10071):815-822. doi:10.1016/s0140-6736(16)32401-1
[3] https://www.mayoclinic.org/diseases-conditions/prostate-cancer/diagnosis-treatment/drc-20353093
[4] Hale GR, Czarniecki M, Cheng A, et al. MP26-08 comparison of elastic and rigid registration during magnetic resonance imaging/ultrasound fusion-guided prostate biopsy. The Journal of Urology. 2018;199(4S):e338-e339. doi.org/10.1016/j.juro.2018.02.866
[5] Logan JK, Rais-Bahrami S, Turkbey B, et al. Current status of magnetic resonance imaging (MRI) and ultrasonography fusion software platforms for guidance of prostate biopsies. BJU International. 2013;114(5):641-652. doi.org/10.1111/bju.12593
[6] Hale GR, Czarniecki M, Cheng A, et al. Comparison of elastic and rigid registration during magnetic resonance/ultrasound fusion-guided prostate biopsy: a multi-operator phantom study. The Journal of Urology. 2018;200(5): 1114-1121. doi.org/10.1016/j.juro.2018.06.028
