
The following story is an exerpt from a 2012 article,"Ultrasound Opens New Doors in Robotic Surgery," by Lisa Fratt of Health Imaging.
Since its introduction more than a decade ago, robotic-assisted surgery has stood out as a game-changer. The robotic console provides a robust platform to enable minimally invasive procedures in urologic, cardiothoracic, gynecologic and general surgical procedures. Today, robotic surgery is witnessing an evolution. The most recent surgical ultrasound systems, specifically BK Ultrasound systems for robotic surgery, are ushering in a new level of precision and diagnostic confidence. Intraoperative robotic-assisted ultrasound helps surgeons to perform more complex procedures robotically with potentially improved outcomes, particularly in radical prostatectomy and partial nephrectomy.
Ultrasound Imaging in Evolution
Just as imaging is critical to conventional surgical procedures, it also plays an essential role in robotic-assisted surgery. One of the first-generation solutions is the laparoscopic ultrasound transducer. First-generation probe technology relied on a sonographer or assistant to control the probe.
“The surgeon needs ultrasound for these procedures. Intraoperative ultrasound technology is an exciting new device in the armamentarium of tools available to the urologist,” says Ashok K. Hemal, MD, director of the robotic and minimally invasive surgery program at Wake Forest Baptist Medical Center in Winston-Salem, N.C.
James Porter, MD, medical director of robot-assisted surgery at Swedish Medical Center in Seattle, explains, “A laparoscopic surgeon has to adapt when he or she starts performing robotic procedures. [In the first-generation model], the surgeon is no longer at the bedside and has to depend on the bedside assistant to perform ultrasound.”
It was a bit of a delicate dance that hinged on close communication. The surgeon directed the assistant to maneuver the probe through the incision. With each move, the surgeon assessed positioning of the probe and re-directed the assistant as needed. “It was a bit like watching a tennis match,” says Stifelman. The surgeon would stare at the probe on one screen and then shift to review the imaging data on another screen. “It was cumbersome.”
 In March 2011,
In March 2011,
BK Ultrasound introduced a new, leading edge paradigm. The Advanced Robotic Technology solution returns control to the surgeon thanks to intraoperative robotic-assisted ultrasound. The robotic solution is comprised of BK Ultrasound’s Flex Focus 800 ultrasound imaging system and Robotic Drop-In transducer. BK also expanded and improved surgeons’ options with the bk5000 ultrasound system. The premium performance system is ideally suited for surgical procedures.
In addition to returning the probe, and its control, to the surgeon, BK's ultrasound system provides enhanced probe flexibility. “The [first-generation] flexible probe is a nice instrument, but the user is entering [the body] through a fixed port and not always able to gain the optimal angles on the kidney or tumor,” says Porter. These instruments were limited to four degrees of flexion: up, down, right and left.
“With the robotically-controlled probe, the surgeon gains angles because of the wristed capability of the robotic instrument,” Porter explains. The transducer is on a wire that can be dropped in at any angle the surgeon needs.
The advanced capabilities of the Robotic Drop-In transducer are ideally suited for the anatomic contours that surgeons must contend with. “The kidney is a complex 3D structure that does not follow geometrical rules. I can position the drop-in probe at any angle in the kidney to obtain the image I need,” says Monish Aron, MD, co-director of robotic surgery and advanced laparoscopy at University of Southern California (USC) in Los Angeles.
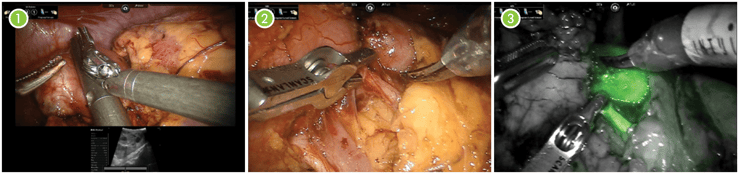
1.) BK probe. Surgeon console view using drop-in probe with Tile-pro. Heads-up display. Tumor seen in ultrasound image. 2.) Placing a miniature robotic bull dog on a tertiary branch of the renal artery. Goal is temporary occlusion of blood supply to tumor and immediate surrounding area while maintaining the rest of kidney perfused. Note the scored capsule just above clamp. Tumor margin identified by using the drop-in BK probe. 3.) Clamp on, indocyanine green (ICG) given fluorescence mode. Green perfused kidney and dark temporary clamped kidney including tumor left of capsule score line. Source: Michael Stifelman, MD
Key In Kidney Care
Partial nephrectomy exemplifies the timeline and impact of the robotic-assisted surgical revolution. Standard laparoscopy may be viewed as the predecessor. The near-microscopic incisions replaced some conventional open procedures and presented a new model, shortening procedure and recovery time. However, there are limits to the surgeon’s ability to perform within the constraints of several minute incisions. Consequently, applications were limited to basic procedures.
Enter first-generation robotic-assisted surgery, which enabled surgeons to regain some dexterity and fine motor control. The slender robotic arms hold instruments, cameras and ultrasound probes and are controlled by the surgeon’s hands. Intraoperative images are ported to the robotic console. Once again, the surgical repertoire expanded to more complex procedures, including partial nephrectomy.
However, there was room for improvement. “Proprioception has been an important part of the surgeon’s toolkit. If the surgeon is working on an organ, he or she can palpate the area with a finger to determine where the artery is. One of the challenges with robotics is that the surgeon no longer feels the tissue,” says Stifelman. Much like the robotic arms allow surgeons to compensate for the reduced dexterity associated with operating through minute incisions, ultrasound enables surgeons to compensate for the lack of proprioception.
“Ultrasound overcomes this challenge and augments what the surgeon can do robotically,” says Stifelman. The surgeon can bring the ultrasound probe into the abdomen any time there is difficulty palpating an organ. In addition to providing clearer visualization and guidance via Doppler imaging, ultrasound also compensates for the loss of proprioception by allowing the surgeon to hear the vessels.
Robotic-assisted partial nephrectomy illustrates these advantages. In fact, in 2010, NYU switched from laparoscopic partial nephrectomies to robotic-assisted procedures. Comparing 120 cases in each group, Stifelman and his team found the robotic procedure was associated with:
- Less blood loss;
- Shorter length of stay; and
- An average 33 percent reduction in the warm ischemia time.
“This technology allows us better outcomes, and allows us to tackle more difficult, complex lesions that we would not have considered for a minimally invasive approach in the past,”
states Stifelman. These include larger tumors, endophytic tumors and tumors close to hilar vessels. Robotic technology scores another clinical point over the laparoscopic option; patient outcomes were worse for complex lesions compared with peripheral lesions when the procedure was performed laparoscopically.
BK Ultrasound’s system plays an essential role throughout the robotic-assisted partial nephrectomy and is critical during several steps in the procedure.
The first step where the BK probe proves its utility is planning the hilar dissection. “It’s really important to identify all of the arteries in the kidney during the hilar dissection,” emphasizes Stifelman. The surgeon needs to isolate the arteries supplying blood flow to the kidney. “The kidneys are highly vascular organs and receive about 1,200 ccs of blood every minute, which is approximately one-fifth of the body’s entire blood volume. If the kidney is perfused and the surgeon makes a cut into the kidney, the patient will bleed profusely and can become hypotensive,” explains Aron of USC.
Urologic surgeons performing partial nephrectomy can use the Robotic Drop-In transducer’s Doppler function to determine the blood supply in the area around the kidney tumor. Aron outlines two options. The surgeon can use a vascular clamp to temporarily interrupt the blood supply to the entire kidney. “The downside to this approach is that there is a finite amount of time that the kidney nephrons can be without blood supply. If it’s a complex tumor, there is a chance that this finite amount of time will be exceeded.”
Another option, says Aron, is selective clamping of the arteries that are supplying blood to the targeted areas of the kidney. The renal arteries branch into secondary, tertiary and quaternary arteries as they get closer to the kidney. “A skilled surgeon can dissect out these smaller branches as they go into the kidney for selective clamping and thereby avoid global kidney ischemia.” The surgeon can then use the drop-in ultrasound probe and its Doppler function to determine whether the target area is still perfused or devoid of blood flow when a small vascular clamp is applied on the appropriate tertiary branch.
Ultrasound also can provide a roadmap to the tumor. “Finding a 1 to 2 cm growth in the kidney can be a bit like finding a needle in a haystack. It’s a 12 to 13 cm organ surrounded by 2 to 3 cm of fat,” says Stifelman. Ultrasound can show the entire kidney and the exact location of the tumor. “Rather than guessing, we can direct our dissection to exactly where the tumor is.” The images are overlaid onto the display, like “picture-in-picture” on a TV screen to guide the surgeon.
The third step in which ultrasound is used in robotic-assisted partial nephrectomy is the verification of tumor margins. Ultrasound provides the depth and margins of the tumor, its lateral location and width as well as the arteries and veins headed to the tumor. With electrocautery, the surgeon can mark the lines of resection on the surface of the kidney. “Finally, when the procedure is finished and the surgeon is ready to close, BK’s technology can be used to confirm that the kidney is being perfused and that nothing has been inadvertently cut,” says Stifelman.
The technology delivers multiple benefits, including increased efficiency, improved patient safety and enhanced diagnostic confidence. “It directs the surgeon where to go and it’s safer because it allows us to clearly mark the lines of demarcation,” says Stifelman, estimating that BK's Robotic probe is 10 times more efficient than earlier models.
Aron of USC adds, “With ultrasound guidance, we are able to excise the tumor and save as much of the kidney as possible.” In fact, the USC team achieves negative margins almost all of the time during robotic-assisted partial nephrectomy. “I use intraoperative ultrasound in every case because it tells the surgeon very clearly where to cut in order to get all the tumor and yet maximize preservation of normal kidney tissue. The only time I did not use ultrasound, I got a positive margin,” shares Aron. Stifelman agrees that intraoperative ultrasound may help reduce the positive margin rate, and notes NYU’s positive margin rate for robotic-assisted partial nephrectomy is 0.9 percent.
According to Aron, the application of intraoperative ultrasound and robotic-assisted surgery may hold additional benefits for several groups of patients. Take for example elderly patients who have an atherosclerotic plaque in the renal artery. The plaque may be composed primarily of calcium. “When the surgeon applies a clamp on the main renal artery, the plaque may fracture into the renal artery and embolize distally thereby blocking blood supply to the entire kidney. The surgeon might be completing a partial nephrectomy and reconstructing the kidney, but unbeknownst to him or her, by virtue of the plaque rupture, the entire kidney may be dying.” Intraoperative ultrasound after the partial nephrectomy is complete can be very useful to assess blood flow in the remnant kidney and can assuage any doubts about the perfusion of the remaining kidney.
Another smaller patient subset that can benefit from the enhanced visualization afforded by the system is patients who have undergone previous kidney surgeries. “They tend to have lots of adhesions around the renal hilum and it can be difficult to dissect out the vessels if there is dense fibrous scar tissue around them,” says Aron. The surgeon can place the probe on the vena cava, or aorta, and move it laterally toward the kidney to image the renal artery and help direct the surgical dissection appropriately.
Hemal also has leveraged BK technology infrequently in patients undergoing robotic pyelolithotomy to identify and remove secondary kidney stones. Without ultrasound, the surgeon’s imaging toolkit would be limited to pre-operative CT or MR imaging, which cannot be used intracorporeally during surgery.
Peering into The Future of Ultrasound and Robotic Surgery
Robotic-assisted surgery has experienced a decade of dramatic growth, which is poised to continue and accelerate in the coming years. “BK's [connectable] robotic ultrasound technology is going to expand into other areas of surgery for a number of reasons. The technology is intuitive and easy to use. It produces clearer images and provides accurate 3D reconstructions,” predicts Patel, who offers that gynecological procedures such as myomectomy may be a future application, as ultrasound can help surgeons localize myomas.
Stifelman agrees that robotic-assisted ultrasound technology will penetrate into other areas of surgery as robotics moves further into the mainstream. “Sites need to understand the question that needs to be answered by the technology,” he says. For example, in gynecological procedures, surgeons need to accurately identify the ureters because they are at risk of being injured during surgeries. “It’s a need that ultrasound could answer.”
Ultrasound is likely to migrate to robotic-assisted surgery in other specialties, including cardiac surgery, pancreatic surgery and general surgery, Stifelman predicts. Porter points to other pluses of the BK system.
“The probe brings major advantages in that the surgeon no longer relies on an assistant for ultrasound imaging. Imaging capability and flexibility are improved. If an organization is serious and planning on a high volume of robotic-assisted surgery, investing in this technology is the right move.”
Medicine occasionally hosts a perfect marriage of technologies, where the combined benefits to the patient and physician are crystal clear. BK Ultrasound's technology, coupled with robotic consoles, exemplifies this type of union and provides a sound platform today and for the future.
Visit our robotic surgery page to learn more about BK's ultrasound systems and transducer for robotic assisted surgery.
*VFI is not licensed by Health Canada and is FDA cleared for the Ultraview 800.

