Dr. Fran Martinez Ricarte is the Coordinator of Neuro-Oncology and Radiosurgery at the Neurosurgery Service of Vall d’Hebrón University Hospital in Barcelona, Spain. He is a member of the Research Unit of Neurotraumatology and Neurosurgery at the Vall d’Hebron Institute of Research.
Case Introduction
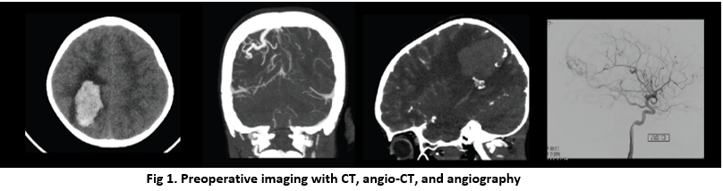
A 6-year-old male patient presented at Vall d’Hebron with a headache that had lasted six days. CT scans, angio-CT scans, and angiography revealed that the patient had a 23 cc parietal hematoma due to a ruptured AVM (Spetzler- Martin Grade 2) [See figure 1]. The surgical approach was chosen to treat the AVM and at the same time evacuate the hematoma. Vascular Neurosurgeon Dr. Dario Gandara joined the surgery with Dr. Martinez Ricarte.
Visualizing the Hematoma with Intraoperative Ultrasound
Navigation was used to guide placement of the skin incision and craniotomy. Hematoma evacuation and AVM removal were performed with the guidance of the bkActiv intraoperative ultrasound system paired with the Craniotomy Transducer (N13C5).
Active imaging with intraoperative ultrasound was used in conjunction with a microscope. The patient was positioned in the lateral position and fixed with the Mayfield skull clamp. A “C” incision was made in the skin, and a right parietal tailored craniotomy was performed.
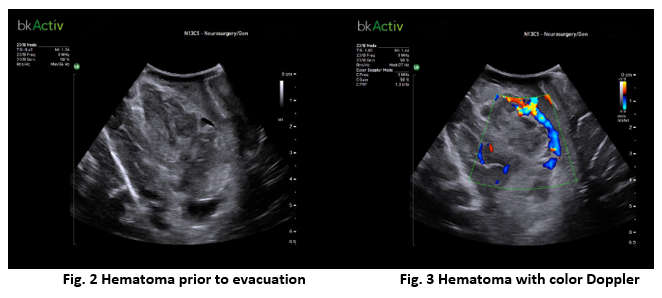
Real-time active imaging was used before opening the dura to visualize the hematoma and the AVM (using color Doppler), and to ensure that the craniotomy would be sufficient in size to expose the entire operative workspace. The surgeons found that the intraoperative ultrasound provided real-time information to check the accuracy of the neuro-navigation intraoperatively and account for brain shift [See figure 2].
The ultrasonographic appearance of hematomas differs depending on the amount of time elapsed since the bleeding occurred. In the acute stage, a hematoma appears hyperechoic, meaning it appears brighter on the ultrasound image than the surrounding tissue and is therefore easy to visualize. As the clotting process progresses, the hematoma becomes progressively more isoechoic, meaning that it more resembles the surrounding tissue.
Resecting the AVM and Evacuating the Hematoma
When the dura was opened, the hematoma and the AVM were visualized using the Craniotomy Transducer directly on the brain tissue. Intraoperative images obtained after opening the dura are more clear than prior to opening the dura.
Color Doppler was activated on the active imaging system to provide more information on the location, size, and flow characteristics of the AVM and the hematoma [See figure 3]. This information was used to decide how to proceed with the resection and evacuation.
After clipping the feeding artery, the nidus was resected and the hematoma evacuated. Active imaging allowed visualization of brain shift due to clot removal and also helped identify the nidus and the abnormal vessels (feeding artery and draining vein).
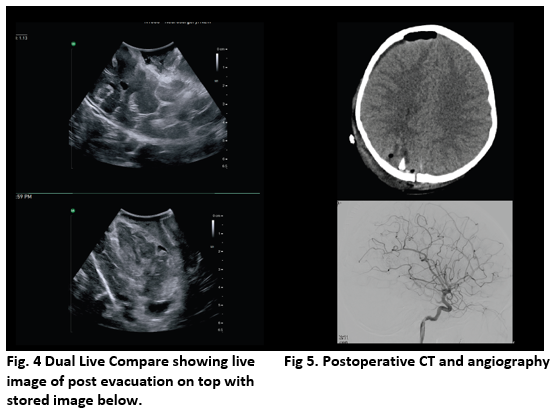
The Dual Live Compare feature was activated on the intraoperative ultrasound system to see the live imaging post evacuation of the hematoma with the baseline scan from before evacuation [See figure 4]. The compare feature allows a fast assessment of the completion of the procedure.
Conclusions
At the end of the surgery, color Doppler was used to make sure that the nidus was completely resected, and there was no visual evidence of flow through the AVM on the intraoperative ultrasound. The procedure was finished by repositioning the bone and fixing it with mini self-tapping plates.
Postoperative CT and angiography were performed to confirm the absence of complications and verify the complete resection of the AVM [figure 5].
In summary, the real-time active imaging was a reliable and useful tool for intraoperative localization and guidance for AVM resection and hematoma evacuation.
