Christopher C. Raio, MD MBA FACEP
Chairman, Department of Emergency Medicine, Good Samaritan Hospital Medical Center, West Islip, NY, USA Progressive Emergency Physicians

A 72 year-old female with a past medical history significant for diabetes and congestive heart failure presented to the emergency department with three days of worsening fatigue. “Mom just has not been acting like herself, and today seems slightly confused at times”, her daughter stated. The day prior, the patient developed a mild, dry cough and fever, with a maximum temperature of 101.2°F (38.4°C). Vital signs on arrival were:
Temperature: 100.5°F (38.1°C)
Pulse: 88 beats/min
BP: 112/76 mmHg
Respirations: 24 breaths/min
Pulse Ox: 95%
On physical examination the patient was alert and oriented, but fatigued with generalized weakness. Other pertinent findings included decreased breath sounds in both lung bases on auscultation, and mild generalized abdominal tenderness without rebound or guarding. Lower extremity edema was not present. Upon review of the electronic medical record, it was noted that a recent echocardiogram revealed an ejection fraction of 30%. The Emergency Medicine physician appropriately initiated treatment via the hospital’s sepsis protocol, ordering appropriate labs including CBC, CMP, troponin, urinalysis, influenza panel, blood and urine cultures, EKG and plain film radiography of the chest. Broad spectrum antibiotics were administered and the pre-determined “checkbox” for an intravenous fluid bolus of 30cc/kg of normal saline was confirmed.
This is a scenario that Emergency Medicine physicians and clinicians encounter every day, and one that provokes heightened debate due to current sepsis guidelines and mandates. One topic of the discussion, - the required large volume fluid administration - is particularly heated. The real issue lies in an inability of clinicians to easily, rapidly, and accurately determine fluid responsiveness in all patients. If this were possible, the decision on whether or not to deliver 30cc/kg would be a simple one, and would come down to who will improve with fluid administration, and who could potentially deteriorate.
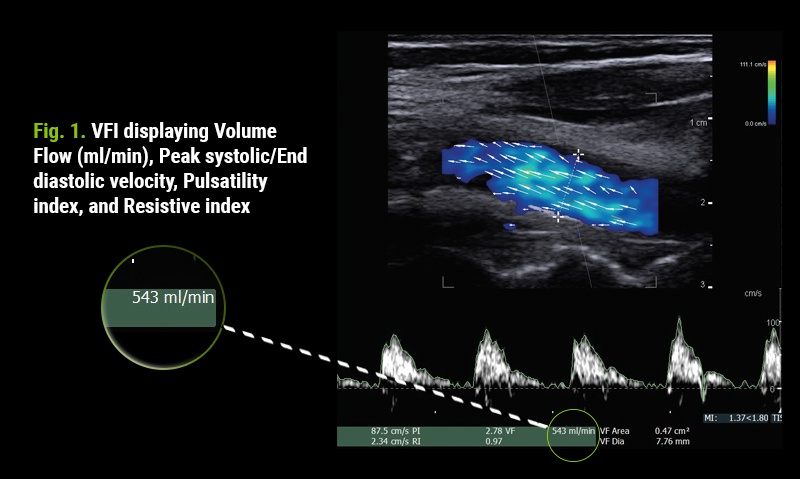
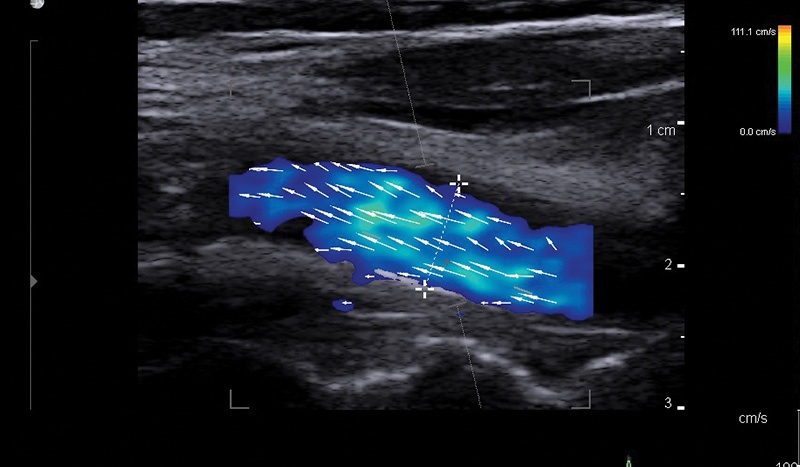
The Emergency Medicine physician circled back to the patient’s bedside. Upon re-evaluation, the concern heightened that overzealous intravenous fluid delivery could tip this patient into worsening heart failure. The bk3500 ultrasound system was brought to the bedside and focused scanning was performed. To no surprise, cardiac windows showed globally decreased contractility, and the inferior vena cava diameter was measured at 1.5 cm with good respiratory variability. The physician then utilized Vector Flow Imaging (VFI) with patented VFI-Volume Flow Assist of the carotid artery to determine real-time volume flow. Within minutes, pre- and post-passive leg raise values of 543 ml/min and 560 ml/min were collected (Fig. 1). This confirmed that the patient was not a fluid responder. The intravenous bolus was canceled and slow maintenance hydration ordered. A urinary tract infection was revealed and the patient responded well to antibiotic therapy and was discharged home on day 3 with no further complications.
Conclusion:
VFI technology allows clinicians to quickly and easily visualize flow direction, presence of laminar versus turbulent flow, flow velocities, and flow volume. VFI-Volume Flow Assist vastly reduces the number of steps necessary to obtain clinically important results. With minimal training, users with varying levels of ultrasound expertise are able to perform the examination and integrate results into positive clinical care. Cumbersome, variable caliper manipulation and angle dependence are eliminated. In this case, the results were utilized to determine fluid responsiveness to avoid fluid overload, or potentially worse, ARDS (Acute Respiratory Distress Syndrome).

