Learn more about how intraoperative ultrasound can influence operative strategy in two-stage liver resections through:
- mapping hepatic vasculature with regards to tumors
- defining margins of resection
- enabling parenchymal-preserving resection
Mathieu D'Hondt, MD
Dept. of Digestive and Hepatobiliary and Pancreatic Surgery, AZ Groeninge Hospital, Kortrijk, Belgium

Liver resection remains the only potentially curative treatment providing long-term survival for patients with extensive bilobar colorectal liver metastases.
A two-stage hepatectomy is a potentially curative strategy that consists of:
• A first-stage procedure, where colorectal liver metastases in one hemiliver are resected. The primary colorectal tumor is often resected by combining a partial colectomy with the first-stage liver resection.
• A second-stage procedure, where all colorectal liver metastases in the contralateral hemiliver are resected.
Apart from a limited number of case studies1,2, the adoption of the laparoscopic approach in a two-stage hepatectomy has not yet been extensively described in literature.
At present, no randomized control trials comparing laparoscopic to open liver resection have been published. However, several studies demonstrate that laparoscopic liver surgery reduces intraoperative blood loss, hospital stay, and morbidity, while maintaining comparable oncological outcomes when compared to open liver surgery3-9.
Case presentation
A 74-year old male presented with weight loss, fatigue, a change in bowel habits (diarrhoea) and abdominal discomfort (cramps). A colonoscopy revealed a large tumor of the sigmoid colon at 30 cm. from the anal verge, with resulting biopsies confirming adenocarcinoma (RAS wild-type).
Preoperative imaging (MRI of the liver) revealed extensive bilobar liver metastases, and the patient was treated with four cycles of combination chemotherapy (FOLFOX) and Cetuximab. New imaging after four cycles of chemotherapy revealed a very good response, and a two-stage hepatectomy was planned during the MDT (Multidisciplinary Team Meeting). During the first stage, the patient underwent a combined laparoscopic sigmoidectomy with clearance of the left hemiliver.
During the procedure, segment-by-segment intraoperative ultrasonography ruled out additional lesions, and lines of transection were marked on the liver’s surface under guidance of intraoperative ultrasound (Fig. 1).
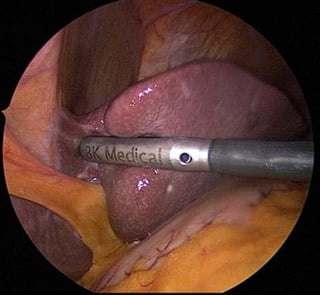
Fig. 1. First stage hepatectomy: a segment-by-segment intraoperative ultrasonography ruled out additional lesions,
and lines of transection were marked on the liver’s surface under guidance of intraoperative ultrasound.
A parenchymal-sparing hepatectomy was performed with a metastasectomy in segment 2, a metastasectomy in segment 3, and a metastasectomy in segment 4B (Fig. 2).
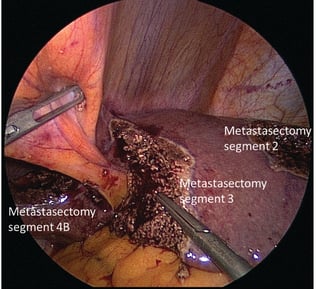
Fig. 2. During the first stage hepatectomy three metastasectomies were performed in
the left hemiliver (1 in segment 2 and 1 in segment 3 and segment 4B).
The post-operative course was uneventful and the patient was discharged on day five post-operatively.
A volumetry of the left hemiliver revealed a volume of 37% and it was not necessary to perform a right portal vein embolisation. Four weeks after the first-step procedure, a laparoscopic right hemihepatectomy was performed. The hepatoduodenal ligament was opened from the cystic duct to the left to identify the right branch of the hepatic artery. The right hepatic artery was clamped using a laparoscopic vascular clamp and patency of the arterial blood supply to the left hemiliver was checked using intraoperative ultrasound. Once the arterial anatomy was clearly identified, the right branch of the hepatic artery was clipped and cut.
The right branch of the portal vein was freed from the adventitional tissue and a right-angled clamp was passed around right portal vein. The bifurcation of the portal vein was also identified.
A vessel loop was passed around the portal vein (Fig. 3), which was clamped with a vascular clamp. Patency of the portal flow to the left hemiliver was assessed using intraoperative ultrasound, and the right portal vein was then clipped and cut. The line of demarcation was seen on the surface of the liver.
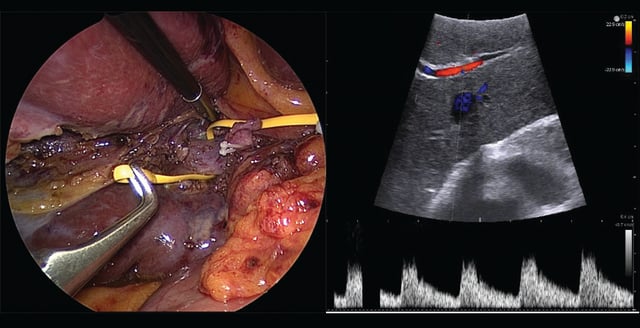 Fig. 3. Laparosopic right hemihepatectomy.
Fig. 3. Laparosopic right hemihepatectomy.
A vessel loop was passed around the portal vein before clipping and transecting the right portal vein.
The right lobe was mobilized by transection of the right coronary ligament and the right triangular ligament, and the short hepatic veins on the right side were divided between clips or ties. The right hepatic vein was prepared at the level of the suprahepatic vena cava, and parenchymal transection was performed using a bipolar Enseal device and CUSA (Cavitron Ultrasonic Surgical Aspirator) (Fig. 4). As a final step, the right hepatic vein was stapled using a vascular stapler.
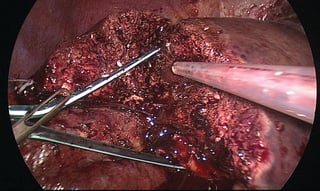 Fig. 4. Laparosopic right hemihepatectomy. Parenchymal transection (hanging manoeuvre).
Fig. 4. Laparosopic right hemihepatectomy. Parenchymal transection (hanging manoeuvre).
The specimen was removed through a Pfannenstiel incision. Adjuvant chemotherapy was started three weeks later (eight cycles in total).
This case-study was performed under approval by the institutional review board and patient consent, and includes only de-identified patient images. The IOUS was performed with a 10-4.3 MHz 4-way laparoscopic transducer and a BK Ultrasound (Peabody, MA) unit.
Conclusion:
A two-stage hepatectomy is a surgical modality recommended for patients with extensive bilobar colorectal liver metastases. Typically, the first step is a parenchymal-preserving liver resection, which can be combined with resection of the primary tumor. The first-stage laparoscopic clearance of one hemiliver could become the gold standard.
Laparoscopic second-stage hepatectomy, which is (mostly) a major hepatectomy, should be limited to selected cases in high-volume HPB (hepatobiliary) centers. Although published data is limited, one of the largest studies published in 201510 showed that laparoscopic two-stage hepatectomy for bilobar colorectal liver metastases is safe, and does not jeopardize long-term outcomes in selected patients.
Despite improvements in preoperative imaging, intraoperative ultrasound remains a valuable tool during the resection of colorectal liver metastases. Compared with cross-sectional preoperative imaging, intraoperative ultrasound is superior in the detection of liver tumors and the planning of surgery11.
-
Intraoperative ultrasound can have an impact on the accurate assessment of the proximity to, or invasion of, the hepatic vasculature. This can influence operative strategy.
-
Intraoperative ultrasound helps the hepatobiliary surgeon to understand the three-dimensional relationship between liver vasculature and tumor.
- Intraoperative ultrasound improves patient outcome by defining adequate margins of resection and selecting the correct type of resection.
- The use of intraoperative ultrasound can modify the operative plan, and may allow a less extensive parenchymal preserving resection to be performed12.
Click here to read more about BK Ultrasound's solution for laparoscopic surgery.
1 Di Fabio F,Whistance R, Rahman S et al. Exploring the role of laparoscopic surgery in two-stage hepatectomy for bilobar colorectal liver metastases. J Laparoendosc Adv Surg Tech A 2012; 22:647–650.
2 Machado MA, Makdissi FF, Surjan RC et al. Two-stage laparoscopic liver resection for bilateral colorectal liver metastasis. Surg Endosc 2010; 24: 2044–2047.
3 McPhail MJ, Scibelli T, Abdelaziz M, et al. Laparoscopic versus open left lateral hepatectomy. Expert Rev Gastroenterol Hepatol. 2009;3:345–351.
4 Parks KR, Kuo YH, Davis JM, et al. Laparoscopic versus open liver resection: a meta-analysis of long-term outcome. HPB. 2014;16:109–118.
5 Mirnezami R, Mirnezami AH, Chandrakumaran K, et al. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and
meta-analysis. HPB. 2011;13:295–308.
6 Cipriani F, Rawashdeh M, Stanton L, et al. Propensity score-based analysis of outcomes of laparoscopic versus open liver resection for colorectal metastases.
BJS. 2016;103:1504–1512.
7 Aldrighetti L, Guzzetti E, Pulitano` C, et al. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results.
J Surg Oncol. 2010;102:82–86.
8 Abu Hilal M, McPhail MJ, Zeidan B, et al. Laparoscopic versus open left lateral hepatic sectionectomy. Eur J Surg Oncol. 2008;34:1285–1288.
9 Abu Hilal M, Di Fabio F, Teng MJ, et al. Single-centre comparative study of laparoscopic versus open right hepatectomy. J Gastrointest Surg. 2011;15: 818–823.
10 Fuks D, Nomi T, Ogiso Set al. Laparoscopic two-stage hepatectomy for bilobar colorectal liver metastases. Br J Surg. 2015 Dec;102(13):1684-90.
11 D’Hondt M, Vandenbroucke-Menu F, Préville-Ratelle S et al. Is intra-operative ultrasound still useful for the detection of a hepatic tumour in the era of modern pre-operative imaging? HPB (Oxford). 2011 Sep;13: 665-9.
12 Knowles SA, Bertens KA, Croome KP et al. The current role of intraoperative ultrasound during the resection of colorectal liver metastases: A retrospective cohort study. Int J Surg. 2015;20:101-6.
