Dr. Stephan Kruck is a senior physician in the Department of Urology at University Hospital Tübingen in southern Germany, an institution renowned for its commitment and dedication to emerging medical technology. Dr. Kruck and his team have been using bkFusion - technology that fuses real-time ultrasound images with pre-exam MRI data – since April 2017.
Fusing real-time ultrasound images with pre-exam MRI data provides better guidance to help accurately target lesions identified on the MRI images, potentially reducing the risk of missing high-grade tumors or under-staging tumors for active surveillance. bkFusion ensures that real- time ultrasound imaging and MRI targets stay aligned with either the free-hand transrectal or the transperineal biopsy approach. Urologists can freely adjust ultrasound gain and depth, or choose to scan in different planes (transverse, sagittal and endfire), without any need for recalibration or loss of alignment before or during procedures. This helps to better target areas of concern.
So far, Dr. Kruck and his team have performed 45 transperineal (TP) procedures with bkFusion.
Dr. Kruck discusses his experiences:
“In general, our bkFusion cases have been on patients with a previous negative 12-core biopsy. The majority of these patients were imaged at our own center with 3T mpMRI imaging.
In the re-biopsy setting, we typically perform between 2 and 6 fusion biopsies, depending on tumor volume, followed by up to 12 systematic biopsies.
We detect prostate cancer in nearly half of all cases, the majority of which is significant prostate cancer. Even after previous negative biopsy we have a very high rate of detection in patients who have high-risk cancer or significant cancer.
The patient in the following case study is 67 years old, and presented with a high PSA level of over 20 ng/ mL. He had one previous negative biopsy, and due to rising PSA levels he underwent a multiparametric MRI (see Fig. 1). The MRI showed a suspicious lesion circumscribed area on the right side of the apical prostate, seen very clearly.
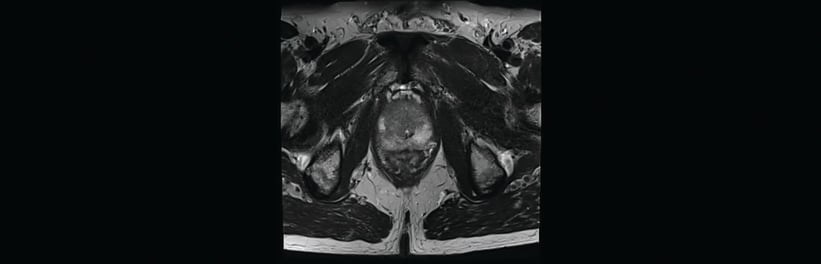 Fig. 1. MRI image showing a suspicious lesion circumscribed area on the right side of the prostate
Fig. 1. MRI image showing a suspicious lesion circumscribed area on the right side of the prostate
I discussed both transperineal and transrectal biopsy approaches with the patient, and we agreed on the 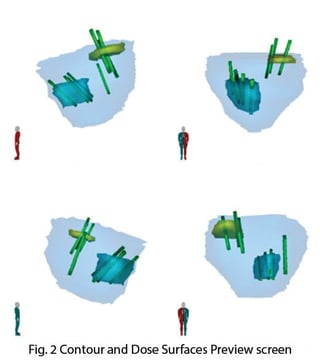 transperineal approach. Many patients are concerned about the rising resistance of bacteria to antibiotics as this is a very hot topic in the media, and patients often know someone who has experienced post-operative infection. After performing around 600 transperineal biopsies, I have only seen one case of infection.
transperineal approach. Many patients are concerned about the rising resistance of bacteria to antibiotics as this is a very hot topic in the media, and patients often know someone who has experienced post-operative infection. After performing around 600 transperineal biopsies, I have only seen one case of infection.
Procedure Steps:
Typically, the patient brings me a CD-ROM with MRI data and the radiology report. After I have contoured the prostate and the suspicious lesions, the data is uploaded to the system.
The next step is to biopsy the lesions. During this particular procedure, I started with the targeted biopsies, and then took the systematic biopsies. bkFusion works with the high-end stepper from CIVCO, which is fully-electronic and linked to the system. The stepper is often used for brachytherapy, so it’s really easy and stable to handle. During the operation, I also have the advantage (via the Predictive Fusion feature) of readapting and reorienting the supine MRI to match the real-time prostate biopsy orientation. I’m not tied to a model on screen that I can’t readjust, and that’s a great benefit.
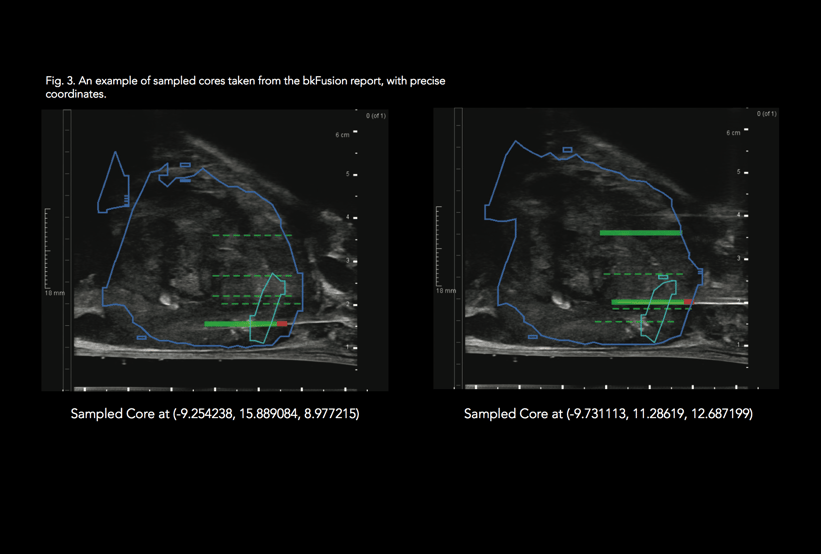
After performing the biopsies, I enter the biopsy positions on the screen. I then click a button to create the report, which I have the option to totally individualize (see Fig. 3). Good documentation is mandatory for treatment planning and active surveillance, and the reports contain a summary of all biopsy procedures, including core number, position, and zone. This makes it very fast to produce a pathology report form.
What’s important for the patient is the detailed cross- sectional drawings of the prostate (see Fig. 2). Patients can understand these drawings, and clearly see their cancer sites and where the biopsies went. I can then explain the implications for surgery.
Results From Pathology:
Pathology results determined significant cancer (Gleason 8 in up to 90% of the core) in all targeted cores.
The summary of findings: PI-RADS 4 (ventral peripheral zone on the right apical and involvement of the apical right anterior transitional zone). No evidence of organ translocation, no pathologically enlarged lymph nodes. The patient will undergo radical prostatectomy.
There’s a real passion for new technology here in Tübingen. This is a center where we look at new ideas, test them, and try to bring them forward.
A major strength of bkFusion is that the system can do both TR and TP procedures in one integrated system, and the benefit for users like university hospitals is that the workflow is virtually the same.”